Managing PBC Symptoms
- Home /
- Managing PBC Symptoms

More than half the people with primary biliary cholangitis do not have any noticeable symptoms when they are first diagnosed. However, symptoms may eventually develop over time.
Patients with PBC may experience some of the following symptoms:
- Fatigue/tiredness – even with adequate sleep
- Pruritus (itching) – occurs all over the body, often on the palms of the hands and soles of the feet- and is not associated with a rash
- Xanthomata (fat deposits under the skin) – small white or yellowish bumps under the skin, especially around the eyes
- Dry eyes, dry mouth
- Bone, muscle, joint pain
- Abdominal pain
If liver disease progresses, some of the more very advanced symptoms may include:
- Ascites (fluid in the abdomen)
- Gastrointestinal bleeding (vomiting blood or passing black bowel movements)
- Jaundice (yellowing of the skin or eyes)
- Hepatic Encephalopathy (confusion associated with liver disease)
It is important to note that worsening severity of these symptoms does not necessarily correlate to worsening disease severity or progression.

Fatigue (tiredness)
Fatigue is the most common symptom of PBC, affecting 70-80% of PBC patients. PBC fatigue is independent of sleep. Someone with PBC fatigue can sleep and wake up “tired”, needing frequent naps during the day. With PBC fatigue completing daily tasks and maintaining social relationships may become challenging. Feelings of social isolation and depression may result and therefore it is important to discuss these symptoms and feeling with your healthcare providers.
With PBC fatigue, your battery (energy) may be running down!
What helps manage fatigue:
- Exercise
- Pace and energy management
- Ask for help and understanding from your family, friends and employer
- Get support
- Start slowly and build up
Fatigue is typically worse later in the day so it may be helpful to plan important activities for the morning when your battery is more fully charged
To rule out other causes of fatigue, listed below, see your primary care provider
- Depression
- Sleep apnea
- Thyroid Disease
- Celiac Disease
- Vitamin D Deficiency
- Anemia
- Pernicious Anemia (Vitamin B12 deficiency)
- Addison’s Disease (Low Cortisol)
- Rheumatologic Conditions

Pruritus (itch)
PBC itch may affect 25-70% of PBC patients and can occur at any stage of disease. This itch is called “cholestatic pruritus”, meaning that it is associated with the bile ducts not working as they should to excrete bile acids. Although the exact cause is unknown, it is thought that the itch may be due to the accumulation of bile acids and other itch-stimulating molecules (known as “pruritogens”) in the blood.
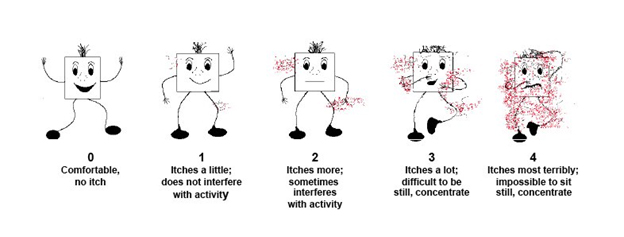
Itch may be experienced differently by each patient. You may track your itch experience noting the following:
- Severity
- Duration
- Time of day
- Part of body
Untreated severe itch may result in:
- Lack of sleep
- Inability to concentrate
- Anxiety/Depression
- Skin infections from scratching
- Social isolation
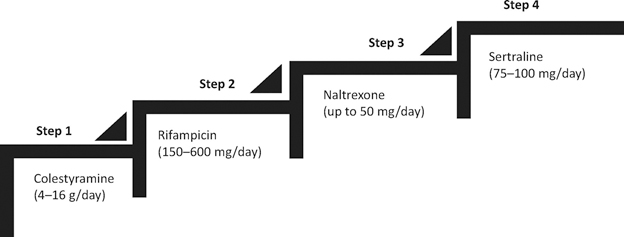
If you are experiencing PBC itch, your specialists may prescribe treatment using a stepped approach.
Apply or Try:
- Topical lotions that contain tannins, camphor or menthol
- Skin moisturizers (unscented, for sensitive skin)
- Non alkaline soaps & lukewarm water
- Wet cold or moist wraps
- Relaxation techniques
- Training to stop the itch, scratch, itch cycle
- Wear loose, breathable clothing
- Drink plenty of water (stay hydrated)
- Use a room humidifier (especially during winter)
Note that not all itching that occurs in patients with PBC is related to their underlying liver disease. Any itching that occurs with a rash is unlikely to be related to the PBC and should be assessed by your physician.